October 20, 2022 – COVID-19 Vaccine-Associated Optic Neuropathy: A Systematic Review of 45 Patients (pdf) “In 2021, vaccination against severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) became a primary focus of public health efforts to control the COVID-19 pandemic. Even though they were generally found to be safe and effective in multiple large controlled clinical trials, the relatively fast and wide deployment of COVID-19 vaccines has made them a subject of considerable scrutiny and analysis since the time of their introduction to the public. The COVID-19 disease itself has affected the eye in many ways. Previous research demonstrated a link between COVID-19 infection and ophthalmic manifestations, both directly and indirectly. For example, it was reported that inflammatory conditions such as conjunctivitis, scleritis, orbital inflammation, keratitis, and retinal affection may be directly linked to COVID-19 infection. Regarding indirect impact, several studies have addressed the relationship between eye strain and dry eye symptoms and the increased screen time in both pediatric and adult populations during the pandemic.”
October 17, 2022 – Ethnicity-Specific Effects on Cardiac Arrest During the COVID-19 Pandemic: A Two-Year Prospective Evaluation in a North American Community (pdf) “The U.S. Hispanic population has experienced a higher incidence of COVID-19 than the NonHispanic White population with disproportionate increases in overall cardiovascular mortality during the pandemic. However, there is a lack of information regarding pandemic-related changes in SCA incidence among Hispanics. In an earlier study conducted pre-pandemic, we reported that Hispanic and Non-Hispanic White residents of Ventura County, CA had similar age-standardized incidence of SCA. In the present analysis, we evaluated incidence of and survival from SCA among Hispanic and non-Hispanic individuals in Ventura County, CA during two years of the COVID-19 pandemic.”
October 1, 2022 – A Case Report: Multifocal Necrotizing Encephalitis and Myocarditis after BNT162b2 mRNA Vaccination against COVID-19 “Although there was no history of COVID-19 for this patient, immunohistochemistry for SARS-CoV-2 antigens (spike and nucleocapsid proteins) was performed. Surprisingly, only spike protein but no nucleocapsid protein could be detected within the foci of inflammation in both the brain and the heart, particularly in the endothelial cells of small blood vessels. Since no nucleocapsid protein could be detected, the presence of spike protein must be ascribed to vaccination rather than to viral infection. The findings corroborate previous reports of encephalitis and myocarditis caused by gene-based COVID-19 vaccines.”
September 7, 2022 – Cardiomyopathy following COVID-19 vaccination in a patient with systemic lupus erythematosus “In this young woman with a long-standing history of SLE, we considered multiple aetiologies forher new onset cardiomyopathy, including ischemic cardiomyopathy, flare of SLE, viral myocarditis, and perimyocarditis following mRNA-based COVID-19 vaccination.”
September 6, 2022 – Myocarditis following COVID-19 vaccine: incidence, presentation, diagnosis, pathophysiology, therapy, and outcomes put into perspective. A clinical consensus document supported by the Heart Failure Association of the European Society of Cardiology (ESC) and the ESC Working Group on Myocardial and Pericardial Diseases “Although generally very safe, post-vaccine myocarditis can result from adaptive humoral and cellular, cardiac-specific inflammation within days and weeks of vaccination. Rates of vaccine-associated myocarditis vary by age and sex with the highest rates in males between 12 and 39 years. The clinical course is generally mild with rare cases of left ventricular dysfunction, heart failure and arrhythmias.”
August 19, 2022 – Safety Monitoring of Pfizer-BioNTech COVID-19 Vaccine Booster Doses Among Children Ages 5-11 Years – United States, May 17-July 21, 2022 “No VAERS reports of myocarditis after third doses among children aged 5–11 years were received. Among children and adolescents aged <18 years, myocarditis risk after COVID-19 vaccination is higher in males (4), and risk decreases with decreasing age (4,8); the myocarditis reporting rate to VAERS after dose 2 was 2.6 per 1 million doses among boys aged 5–11 years and 46.4 per 1 million doses among males aged 12–15 years (8). The risk for myocarditis after dose 3 appears to be less than that after dose 2; among males aged 12–15 years, the reporting rate to VAERS after dose 3 (15.3 per 1 million doses) was approximately one third of that after dose 2.
August 12, 2022 – Tolerability of COVID-19 Infection and Messenger RNA Vaccination Among Patients With a History of Kawasaki Disease “The COVID-19 cohort included 37 patients (mean [SD] age, 11.0 [5.5] years; 22 male [59.5%]). No patients required hospitalization due to COVID-19. The most common symptoms included low-grade fever, fatigue, cough, and myalgia with resolution within a few days. Two patients, aged 9 and 19 years, had extended cough and fatigue for 3 to 4 weeks. One patient developed COVID-19 within 6 weeks of receiving intravenous immunoglobulin for KD.
August 7, 2022 – Cardiovascular Effects of the BNT162b2 mRNA COVID-19 Vaccine in Adolescents “Data including demographics, symptoms, vital signs, ECG, echocardiography and cardiac enzymes were collected at baseline, Day 3, Day 7, and Day 14 (optional) using case record forms. We enrolled 314 participants; of these, 13 participants were lost to follow up, leaving 301 participants for analysis. The most common cardiovascular effects were tachycardia (7.64%), shortness of breath (6.64%), palpitation (4.32%), chest pain (4.32%), and hypertension (3.99%). Seven participants (2.33%) exhibited at least one elevated cardiac biomarker or positive lab assessments. Cardiovascular effects were found in 29.24% of patients, ranging from tachycardia, palpitation, and myopericarditis. Myopericarditis was confirmed in one patient after vaccination. ”
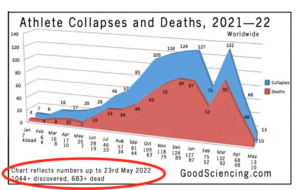
May 21, 2022 – 1024 Athlete Cardiac Arrests, Serious Issues, 666 Dead, After COVID Shot “The deaths of young high level athletes continues. Prior to the mRNA/LPN platform, it was a rare event to see a young athlete perish on the pitch. We’re seeing it multiple times per week. Lipid nanoparticles can penetrate tight junctions. Exercise loosens tight junctions around in the coronary vessels.”
May 18, 2022 – Association of Cerebral Venous Thrombosis with mRNA COVID-19 Vaccines: A Disproportionality Analysis of the World Health Organization Pharmacovigilance Database “Our study has limitations. First, if the national drug-monitoring center of a country does not report ADRs, these cases will not be present in VigiBase. However, VigiBase includes rare ADRs and generalized ADR information from more than 130 countries. Second, VigiBase does not provide any validation of laboratory findings, radiologic information, or accuracy of diagnosis. Information on whether CVT occurred after the first or the second vaccine dose was also not included. Third, vaccine-induced immune thrombotic thrombocytopenia received major public attention after April 2021, and this may have affected the increased reports of CVT cases after COVID-19 vaccination. Lastly, as mentioned above, it is difficult to directly compare outcome parameters, including death, between the different types of COVID-19 vaccines in VigiBase.”
May 15, 2022 – Flare-up of generalized pustular psoriasis combined with systemic capillary leak syndrome after coronavirus disease 2019 mRNA vaccination “There are few reports on CVT after mRNA-based COVID-19 vaccination. These studies suggested that CVT occurrences related to mRNA-based COVID-19 vaccines may be due to endothelial dysfunction caused by spike glycoprotein interactions with endothelial cells resulting in immunothrombosis. If the spike glycoprotein of mRNA-based COVID-19 vaccines binds to the angiotensin-converting enzyme 2 receptor, several inflammatory and thrombogenic molecules, such as leukocyte chemotactic factors, cell adhesion molecules (vascular cell adhesion molecule 1 and intercellular adhesion molecule 1), and procoagulant cytokines, can be activated. This mechanism may cause endothelial dysfunction, particularly in brain endothelial cells, which could contribute to a significant disruption of brain endothelial barrier integrity, ultimately promoting thrombus formation.”
April 29, 2022 – Fatal cerebral haemorrhage after COVID-19 vaccine “A few days after this incident, Oslo University Hospital, Rikshospitalet reported multiple cases of severe blood clots and bleeding in patients who had received an identical vaccine. These patients also had low platelet counts, and in these cases a link was found between the events and the vaccine. Since then, the condition has been referred to as vaccine-induced immune thrombotic thrombocytopenia (VITT), which is characterised by low platelet counts, thrombus formation and antibodies to PF4. In light of this knowledge, new investigations were carried out, and our patient was also found to have a tendency towards thrombus formation with small thrombi in the transverse sinus, frontal lobe and pulmonary artery.
April 8, 2022 – Cardiac Complications After SARS-CoV-2 Infection and mRNA COVID-19 Vaccination — PCORnet, United States, January 2021–January 2022 – Using electronic health record (EHR) data from 40 U.S. health care systems during January 1, 2021–January 31, 2022, investigators calculated incidences of cardiac outcomes (myocarditis; myocarditis or pericarditis; and myocarditis, pericarditis, or MIS) among persons aged ≥5 years who had SARS-CoV-2 infection, stratified by sex (male or female) and age group (5–11, 12–17, 18–29, and ≥30 years). … The incidence of myocarditis or pericarditis in this risk window was 0, 8.1, 8.1, 9.5 cases per 100,000 for females 5-11, 12-17, 18-29, and ≥30 years after a first dose of an mRNA COVID-19 vaccine; 0, 7.5, 5.8, and 8.0 cases per 100,000 after a second dose; 0, 6.7, 12.9, and 14.2 cases per 100,000 after an unspecified dose; and 0, 7.5, 8.7, and 10.1 cases per 100,000 after any dose.”
March 25, 2022 – Persistent Cardiac Magnetic Resonance Imaging Findings in a Cohort of Adolescents with Post-Coronavirus Disease 2019 mRNA Vaccine Myopericarditis – “This was explained as immune-mediated coagulopathy that can also cause arterial thrombosis, which often affects multiple arterial territories, although small-artery stroke is less common. VITT has been described more frequently with the adenovirus vector vaccine. For the moment, there is only 1 report, by Sangli and colleagues, who describe a catastrophic thrombosis after a second dose of the Moderna SARS-CoV-2 messenger RNA (mRNA) vaccine. However, antibodies against PF4 were not determined in our cases; hence this pathogenic mechanism cannot be completely ruled out.”
February 15, 2022 – Myocardial Injury Pattern at MRI in COVID-19 Vaccine–associated Myocarditis “Twenty-one patients (23%) had COVID-19 vaccine associated myocarditis, of which 17 (81%) were male and mean (SD) age was 31 years; 10 (11%) had myocardial injury following COVID-19 illness and 61 (66%) had myocarditis not temporally associated with either COVID-19 vaccination or COVID-19 illness (non-COVID-19 viral/post-infectious in 19 [31%], autoimmune in 8 [13%], drug related in 6 [10%], hyper-eosinophilic in 3 [5%], and other/unknown in 25 [41%]). Patients with vaccine associated myocarditis were younger and more frequently male compared to the other groups. The median [IQR] interval between symptom onset and MRI was 11 [4-29] days.”
February 14, 2022 – Autopsy Histopathologic Cardiac Findings in Two Adolescents Following the Second COVID-19 Vaccine Dose “We report the autopsy results including microscopic myocardial findings of two teenage boys who died within the first week after receiving the second Pfizer-BioNTech COVID-19 dose. The microscopic findings are not the alterations seen with typical myocarditis. This suggest a role for cytokine storm which may occur with an excessive inflammatory response, as there also is a feedback loop between catecholamines and cytokines
February 12, 2022 – Acute Pericarditis Post mRNA-1273 COVID Vaccine Booster “In addition, an increased risk of myocarditis and pericarditis has been reported following mRNA vaccinations, particularly in adolescent males. A September 2021 systematic review of the literature analyzed 69 available case reports and case series of cardiac complications following mRNA vaccinations and found that out of 243 patients, 227 were diagnosed with myocarditis/ myopericarditis, and seven were diagnosed with pericarditis. The majority (92%) were males, and the mean age was 21 years (range, 12-70 years). Three-quarters of the patients who were diagnosed with myocarditis or pericarditis had received the BNT162b2 vaccine (Pfizer-BioNTech), and most (88%) were diagnosed after the second vaccine dose, with a median time from immunization to symptom onset of three days (range: 1.5 hours to 73 days)”
February 7, 2022 – Long-term cardiovascular outcomes of COVID-19 “Because some COVID-19 vaccines might be associated with a very rare risk of myocarditis or pericarditis, and to eliminate any putative contribution of potential vaccine exposure to the outcomes of myocarditis and pericarditis in this study, we conducted two analyses. First, we censored cohort participants at the time of receiving the first dose of any COVID-19 vaccine. Second, we adjusted for vaccination as a time-varying covariate. Both analyses were conducted versus both the contemporary and historical control groups. The results suggested that COVID-19 was associated with increased risk of myocarditis and pericarditis in both analyses.
January 25, 2022 – Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021 “Of the 1991 reports of myocarditis, 1626 met the CDC’s case definition for probable or confirmed myocarditis (Table 1). There were 208 reports that did not meet the CDC’s case definition for myocarditis and 157 reports that required more information to perform adjudication (eTable 3 in the Supplement). Of the 1626 reports that met the CDC’s case definition for myocarditis, 1195 (73%) were younger than 30 years of age, 543 (33%) were younger than 18 years of age, and the median age was 21 years (IQR, 16-31 years) (Figure 1). Of the reports of myocarditis with dose information, 82% (1265/1538) occurred after the second vaccination dose.”
December 19, 2021 – Cardiovascular and haematological events post COVID-19 vaccination: A systematic review “Two hundred and seventeen individuals who received AstraZeneca vaccine experienced 747 CV and haematological events as some of them suffered from multiple events (74 cardiac problems, 375 thrombosis, 206 TP and 92 haemorrhage). Sixty-one events were experienced by 21 individuals who received the J&J vaccine (one cardiac, 40 thrombosis and 20 TP). A total of two cases experienced CV and haematological events following receiving the CoronaVac vaccine (one Kounis Syndrome, Type I variant and 1 haemophagocytic lymphohistiocytosis). As several individuals experienced multiple events.”
December 2, 2021 – Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel “Among 304 persons with symptoms of myocarditis, 21 had received an alternative diagnosis. Of the remaining 283 cases, 142 occurred after receipt of the BNT162b2 vaccine; of these cases, 136 diagnoses were definitive or probable. The clinical presentation was judged to be mild in 129 recipients (95%); one fulminant case was fatal. The overall risk difference between the first and second doses was 1.76 per 100,000 persons (95% confidence interval [CI], 1.33 to 2.19), with the largest difference among male recipients between the ages of 16 and 19 years (difference, 13.73 per 100,000 persons; 95% CI, 8.11 to 19.46).”
December 2, 2021 – Myocarditis after Covid-19 Vaccination in a Large Health Care Organization “A total of 76% of cases of myocarditis were described as mild and 22% as intermediate; 1 case was associated with cardiogenic shock. After a median follow-up of 83 days after the onset of myocarditis, 1 patient had been readmitted to the hospital, and 1 had died of an unknown cause after discharge. Of 14 patients who had left ventricular dysfunction on echocardiography during admission, 10 still had such dysfunction at the time of hospital discharge. Of these patients, 5 underwent subsequent testing that revealed normal heart function.
November 8, 2021 – Abstract 10712: Mrna COVID Vaccines Dramatically Increase Endothelial Inflammatory Markers and ACS Risk as Measured by the PULS Cardiac Test: a Warning “At the time of this report, these changes persist for at least 2.5 months post second dose of vac. We conclude that the mRNA vacs dramatically increase inflammation on the endothelium and T cell infiltration of cardiac muscle and may account for the observations of increased thrombosis, cardiomyopathy, and other vascular events following vaccination.”
October 30, 2021 – Cardiovascular Complications of COVID-19 Vaccination “MI in response to vaccine (Kounis syndrome) has been implicated as one possible mechanism; vaccine induced immune thrombosis with thrombocytopenia (VITT) has been reported as the cause in an another instance. In this context, for acute CV diseases, such as acute MI, acute heart failure or exacerbation of chronic heart failure, vaccination should be postponed until the patient is in a stable condition. In addition to myocarditis and possible MI, post vaccination pericarditis, vasculitis, and cardiac arrhythmia in patients with good general past health after mRNA vaccination have also been reported for both Pfizer and Moderna vaccines.”
October 15, 2021 – Shedding the Light on Post-Vaccine Myocarditis and Pericarditis in COVID-19 and Non-COVID-19 Vaccine Recipients “Myocarditis can reduce the heart’s ability to function or cause arrhythmia CDC. Currently, there are increasing numbers of adverse even reports of post-COVID-19 myocarditis and pericarditis. Pericarditis is inflammation of the fibro-serous sac surrounding the heart (pericardium) from various origins, such as infection, neoplasm, autoimmune process, injuries, or drug-induced according to MeSH Descriptor Data 2021. Pericarditis usually leads to pericardial effusion or constrictive pericarditis.
October 2021 – Diffuse Thromboses in a 2-year-old With Sepsis and Respiratory Failure “Other respiratory viruses including influenza B, parainfluenza and respiratory syncytial virus have been shown to similarly activate the extrinsic coagulation system via tissue factor. Although this patient’s case, which occurred in March 2019, preceded the global pandemic, certainly SARS-CoV-2 and Multisystem Inflammatory Syndrome in Children would now be at top of the differential diagnosis. Macro and microvascular thrombotic complications are associated with severe presentations of COVID-19 in adult patients, including pulmonary embolisms, deep venous thromboses and diffuse microvascular angiopathic complications detected on autopsies. Similar to the pathogenesis of influenza-associated thrombosis, SARS-CoV-2 is thought to activate the coagulation pathway indirectly by producing endothelial injury. SARS-CoV-2 enters endothelial cells through the ACE2 receptors which through complex pathways stimulates aggressive cytokine release and subsequent activation of the extrinsic clotting cascade via tissue factor. ”
September 30, 2021 – Case Report: ANCA-Associated Vasculitis Presenting With Rhabdomyolysis and Pauci-Immune Crescentic Glomerulonephritis After Pfizer-BioNTech COVID-19 mRNA Vaccination “Interestingly, four cases of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) presenting with pauci-immune crescentic glomerulonephritis (GN) after COVID-19 mRNA vaccination have already been reported.”
August 23, 2021 – Suspected Cardiovascular Side Effects of Two COVID-19 Vaccines “A total of 4,564 cases of thrombotic/embolic events (2.04% of all individual cases) were reported after vaccination with Tozinameran (Table3). These include 2,778 thrombosis cases with 84 deaths (3%) and 1,786 embolism cases, which were fatal in 155 (8.7%) vaccinated persons. Most of the embolism cases (91.8%) involved the lungs (n=1,639). Of these affected, 8.9% (n=146) died. Peripheral hemorrhages were slightly more common than central hemorrhages (n=523), but less dangerous (7.5% fatal). Inflammatory changes in the vessels were observed more frequently than in the CNS. They resulted in a comparatively low fatality rate (2.3%). Ischaemic conditions, vascular occlusions and stenoses occurred approximately equally often compared to central disorders (0.05%-0.07%) and were also similarly serious (13%-18% fatalities). Increased blood coagulation was reported in 221 individual laboratory reports (0.1% of all individual cases); 9% were fatal. The proportion of increased D-dimer was only 131 cases associated with a 3.8% fatal outcome.”
August 6, 2021 – Myocarditis and pericarditis after mRNA COVID-19 vaccination in children: Interim guidance (pdf) “Since April 2021, there are increasing reports of cases of myocarditis and pericarditis after mRNA COVID-19 vaccination (Pfizer-BioNTech BNT162b2 vaccine and Moderna mRNA-1233 vaccine).1-5 In Canada, there have been a small number of these reports. 6-8 The Public Health Agency of Canada (PHAC), Health Canada and Public Health Ontario (PHO) are closely monitoring these rare events, including those among youth. To date, PHO has received reports of a number of cases of myocarditis/pericarditis in the 12 to 17 age group in Ontario through the provincial surveillance of Adverse Event Following Immunization (AEFI). The Centers for Disease Control (CDC) in the United States have also reported an increased risk of myocarditis and pericarditis in the 7 days after receipt of dose 1 or dose 2 of an mRNA COVID-19 vaccine, particularly among younger males after dose 2.
August 6, 2021 – Cerebral venous thrombosis after vaccination against COVID-19 in the UK: a multicentre cohort study “Between December 20, 2020, and May 24, 2021, a total of 2,558,421 Clalit Health Services members received at least one dose of the BNT162b2 mRNA Covid-19 vaccine; of these patients, 2,401,605 (94%) received two doses. Initially, 159 potential cases of myocarditis were identified according to ICD-9 codes during the 42 days after receipt of the first vaccine dose. After adjudication, 54 of these cases were deemed to have met the study criteria for a diagnosis of myocarditis. Of these cases, 41 were classified as mild in severity, 12 as intermediate, and 1 as fulminant.”
August 2, 2021 – Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 Vaccination “As part of their open ’Yellow Card’ reporting, the UK Medicines and Healthcare Products Regulatory Agency (Department of Health and Social Care) have listed the incidence of suspected myocarditis and pericarditis after receiving the Pfizer/BioNTech vaccine (81 myocarditis, 63 pericarditis), and Moderna (9 myocarditis, 9 pericarditis, 1 endocarditis), with an incidence of 5.0 per million doses.
July 31, 2021 – Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vaccination-associated autoimmune myocarditis? “Beyond casual mild to moderate post-vaccination side effects that normally disappear within a few hours/days, some other rare adverse effects such as cerebral venous sinus thrombosis, acute ST-segment elevation myocardial infarction (STEMI) with large thrombus in coronary arteries as well as (autoimmune) myocarditis have also been reported recently. We would like to present the findings of three different patients that presented to our hospital until mid of June 2021 and showed unusual serious adverse cardiovascular events of infarct-like myocarditis (in the absence of CAD), possibly linked to preceding COVID-19 vaccination. CMR imaging revealed some interesting patterns of myocardial damage suggestive of “autoimmune” myocarditis that show some minor differences to the well-known CMR pattern of “viral” myocarditis.”
July 28, 2021 – Isolated Tachycardia Presenting After Pfizer-BioNTech COVID-19 Vaccination “We present the first documented case of tachycardia and palpitations, in the absence of other signs or symptoms, presenting within hours of receiving the Pfizer-BioNTech COVID-19 vaccination. Clinicians should be aware that this appears to be benign and resolved within 24 hours in our patient.”
July 27, 2021 – Cardiovascular Adverse Events Reported from COVID-19 Vaccines: A Study Based on WHO Database “The Case Series Drug Analysis Print published by Pfizer-BioNTech for their COVID-19 vaccine as of May 28, 2021, reported a total of 2342 cardiac AEs, among which 1098 events were of palpitation, 466 events of tachycardia, 108 events of atrial fibrillation, 94 events of myocardial infarction, 62 events of cardiac arrest, 63 events of cardiac flutter, 32 events of sinus tachycardia, 46 events of angina pectoris, 24 events of cardiac failure, 38 events of arrhythmia and 16 events of acute myocardial infarction.”
June 16, 2021 – Myocarditis Temporally Associated With COVID-19 Vaccination “Myopericarditis has been reported as a rare vaccination complication.3 We present a case series of 7 patients hospitalized for acute myocarditis-like illness after COVID-19 vaccination, from 2 US medical centers in Falls Church, VA, and Dallas, TX. All were men <40 years of age and of White or Hispanic race/ethnicity. Six patients received an mRNA vaccine (Moderna or Pfizer/BioNTech), and 1 received the adenovirus vaccine (Johnson and Johnson).”
June 2, 2021 – Transient Cardiac Injury in Adolescents Receiving the BNT162b2 mRNA COVID-19 Vaccine “All patients were males and 16–18 years of age, of Jewish descent, that presented with chest pain beginning 1–3 days following vaccination (mean 2.1 days). In 6 of the 7 patients, symptoms began after the 2nd dose and in 1 patient after the 1st dose. Notable abnormal findings in these cases include elevated troponin levels averaged 3538 nanogram/L (range 252–13,720 nanogram/L), ECG changes consistent with pericarditis or myocarditis (6/7 cases) and abnormal findings in echocardiography predominantly pericardial effusion (3/7 cases).”
January 9, 2021 – SARS-CoV-2 Spike Protein Elicits Cell Signaling in Human Host Cells: Implications for Possible Consequences of COVID-19 Vaccines (full text) “PAH is a serious disease without a cure that can affect males and females of any age including children. The increased pulmonary vascular resistance in PAH results in right heart failure and subsequently death. Patients diagnosed with PAH only live for 2–3 years from the time of diagnosis on average if untreated.”
September 6, 2020 – Effects of treadmill exercise on the regulation of tight junction proteins in aged mice “Also, zonula occluden-1 (ZO-1) protein expression level was not significant difference among all mice group. In addition, old mice group had higher level of serum LPS compared to young mice group, but the level was downregulated in both 2 months and 21 months mice group after four weeks of treadmill exercise. Zonulin, which is known as degrading tight junction protein, is not significantly changed by both age and exercise.”